
Table des matières
Conduit électrique plays a fundamental role in the safe and reliable operation of health care facilities. Whether it’s a large hospital, an intermediate care facility, or a community medical center, properly installed conduit ensures that electrical wiring is protected, organized, and compliant with code requirements.
In these environments, the electrical system supports everything from lighting and life-support equipment to data networks and HVAC controls. Electrical conduit, especially types like PVC electrical conduit that helps shield these systems from physical damage, moisture, and interference, while also allowing for efficient installation and maintenance.
This article will explore the importance of electrical conduit in health care settings, common types used, considerations for installation, and how conduit systems support the work of electrical and mechanical engineers, contractors, and facility managers alike.
After reading this article, you’ll know:
- What is electrical conduit and the types for health care facilities
- What is health care facilities and types
- Codes requirements for electrical conduit in health care facilities
- Installation and maintenance of electrical conduit in health care facilities
Qu'est-ce qu'un conduit électrique ?
An electrical conduit is a protective tubing system used to route and safeguard electrical wiring in buildings and structures. It serves two main purposes: mechanical protection of the wires and compliance with safety regulations. Conduits are typically installed in walls, ceilings, floors, or underground to contain insulated conductors, prevent accidental damage, and maintain an organized, code-compliant electrical system.
In health care settings, electrical conduit systems are essential for safely distributing power to critical equipment, emergency lighting, HVAC systems, and mechanical equipment. They also help meet the rigorous code requirements related to fire protection, patient safety, and continuity of service.
A well-designed conduit system in a hospital or clinic ensures the electrical infrastructure remains safe, accessible, and adaptable, which are the factors that especially important in facilities where even minor electrical failures can affect patient care.
7 Common Conduit Types Used in Health Care Facilities
In health care facilities, electrical conduit systems must meet strict safety, hygiene, and reliability standards. Selection is based not just on location and environment, but also on compliance with the National Electrical Code (NEC) Article 517, which governs wiring in patient care areas, critical branches, life safety systems, and essential electrical systems.
Conduit types used are broadly categorized into metallic and non-metallic, and their selection depends on mechanical protection needs, grounding requirements, fire ratings, moisture exposure, and ease of future maintenance.
Metallic Conduit Types

Metallic conduit systems are commonly used in patient care spaces, mechanical rooms, and fire-rated assemblies, primarily due to their grounding continuity, mechanical strength, and fire resistance.
• EMT (Electrical Metallic Tubing)
Widely used in indoor health care applications, including patient rooms, procedure rooms, and general hospital corridors.
EMT is permitted in patient care areas when properly bonded and secured.
Avantages :
Léger et facile à plier
Provides a continuous grounding path
Fire-resistant
Limites:
Must be used with listed fittings and bushings
Not recommended for corrosive or wet environments without extra protection
• IMC (Intermediate Metal Conduit)
Applied in areas requiring higher impact resistance than EMT, such as service entrances or exposed mechanical spaces.
Avantages :
Thicker wall than EMT
Approved for indoor and outdoor installations
Can be used in place of RMC to reduce cost and weight
Limites:
Heavier and more rigid than EMT
Requires threading tools if not pre-threaded
• RMC (Rigid Metal Conduit)
Essential in critical areas exposed to mechanical stress or moisture, including generator rooms, rooftop installations, and underground raceways.
RMC is permits in all health care settings; it provides the highest level of physical protection.
Avantages :
Maximum durability
Excellent for grounding
Corrosion resistance (when galvanized)
Limites:
Heavy and more labor-intensive
Requires threading and specialized tools
• LFMC (Liquid-tight Flexible Metal Conduit)
Used to connect vibrating or movable equipment like HVAC units, motors, or pumps in mechanical rooms.
Not generally used as a primary raceway in patient care areas. Limited use permitted where flexibility is essential.
Avantages :
Waterproof jacket
Flexible routing
Limites:
Short runs only
Must be bonded and terminated properly
Non-Metallic Conduit Types
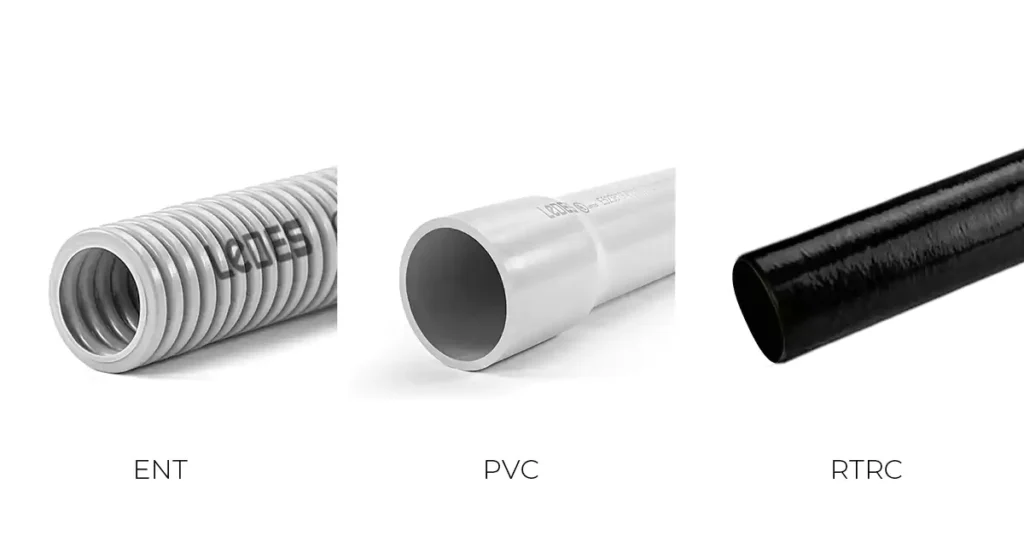
Non-metallic conduits are used more selectively in health care environments, typically in non-patient areas, underground runs, or locations where corrosion is a major concern. Their usage is more restricted inside patient care spaces due to grounding requirements under NEC.
• PVC Conduit (Rigid Nonmetallic Conduit – RNC)
PVC conduit (RNC) commonly used for underground feeder conduits, outdoor lighting, and utility services outside the building envelope.
Not allowed in patient care spaces unless installed in listed metal raceways or systems that provide redundant ground paths.
Avantages :
Lightweight and corrosion-resistant
Rentable
Easy to cut and solvent weld
Limites:
Requires proper solvent welding and curing
Not suitable for plenum spaces or critical branch circuits without additional protection
• ENT (Electrical Nonmetallic Tubing)
Used behind walls or ceilings in non-patient care areas, such as administration, offices, or residential quarters.
tubulure ORL is not permitted in patient care areas per NEC 517.13 due to lack of a continuous grounding path.
Avantages :
Very flexible and fast to install
Uses snap-lock fittings
Limites:
Limited to dry, concealed areas
Cannot be used in fire-rated assemblies unless specifically listed
• RTRC (Reinforced Thermosetting Resin Conduit – Fiberglass)
Rare but valuable in chemical or corrosive environments, such as certain labs or sterilization rooms.
Avantages :
High corrosion and temperature resistance
Non conducteur
Limites:
Higher cost
Requires special adhesive joining and supports
Tableau récapitulatif :
Here are 7 types of electrical conduit used for Health Care Facilities summary list.
Type de conduit | Avantages | Limites | Référence NEC | CEC Reference |
EMT | Lightweight, easy to bend; provides continuous grounding; fire-resistant | Not for wet/corrosive areas unless protected; needs listed fittings | Article 358 | Rule 12-1400 to 12-1414 |
IMC | Thicker wall than EMT; cost-effective vs. RMC; indoor/outdoor use | Heavier than EMT; threading needed | Article 342 | Rule 12-1000 to 12-1014 |
RMC | Highest durability; corrosion resistant; excellent grounding | Heaviest; labor-intensive; threading required | Article 344 | Rule 12-1000 to 12-1014 |
LFMC | Waterproof; flexible routing | Not for long runs; not primary raceway in patient care; proper termination needed | Article 350 | Rule 12-1300 to 12-1308 |
PVC | Lightweight, corrosion-resistant; easy installation; low cost | Not allowed in patient areas; no inherent grounding; solvent welding needed | Article 352 | Rule 12-1100 to 12-1124 |
ORL | Very flexible; fast install; snap-fit fittings | Dry, concealed areas only; no fire rating unless listed; not for patient care | Article 362 | Rule 12-1500 to 12-1514 |
RTRC | High corrosion/temperature resistance; non-conductive | Expensive; special adhesives & supports required | Article 355 | Rule 12-1200 to 12-1220 |
Understanding Health Care Facilities

Health care facilities encompass a wide range of building types, each with distinct functions, patient care needs, and infrastructure requirements. Electrical conduit design within these facilities is not one-size-fits-all, it must be tailored to the specific operational and safety needs of the environment.
To support this, the National Electrical Code (NEC) Article 517 – Health Care Facilities provides detailed rules for electrical systems in medical environments, including specifications for wiring methods, grounding, essential systems, and patient protection.
What Is a Health Care Facility?
A health care facility is any building or part of a building where medical, dental, psychiatric, nursing, or surgical care is provided to individuals. This includes treatment areas where patients may be examined, diagnosed, or cared for, whether for routine outpatient visits or for life-sustaining procedures.
NEC defines patient care spaces as areas intended to be used for treatment or care of patients. These spaces require enhanced electrical protection, including strict conduit and grounding rules, to prevent electrical shock, interference, or failure during critical operations.
6 Common Types of Health Care Facilities
Understanding the facility type helps determine conduit system requirements, particularly in patient care zones. Below are the most common categories:
1. Hospitals
Hospitals are large, complex institutions that provide comprehensive medical services, including emergency care, inpatient treatment, surgery, critical care, diagnostics, and specialty care. They operate 24/7 and must support life-saving interventions, continuous patient monitoring, and rapid response capabilities.
Hospitals typically include:
Emergency departments
Intensive care units (ICUs)
Operating theaters
Patient wards
Diagnostic imaging departments
Laboratories
Pharmacy and sterile processing
Mechanical/electrical service areas
2. Ambulatory Health Care Centers
These facilities offer same-day medical services without requiring overnight stays. They are designed to increase access to care while reducing the strain on hospitals.
Common types include:
Urgent care centers
Dialysis clinics
Day surgery centers
Imaging and diagnostic labs
Outpatient therapy and rehabilitation centers
These facilities prioritize patient flow, efficiency, and quick service delivery in a clean, well-controlled environment.
3. Community Health Clinics and Medical Offices
Serving as the front line of preventive care, these facilities are typically located in neighborhoods or rural areas to provide accessible medical services. They focus on routine health checks, vaccinations, chronic disease management, and family medicine.
4. Skilled Nursing Facilities (SNFs)
SNFs offer round-the-clock care for patients recovering from surgery, illness, or injury who require nursing and rehabilitation services. These facilities bridge the gap between hospital discharge and return to home.
5. Assisted Living and Long-Term Care Facilities
These facilities provide housing and limited medical assistance to elderly individuals or those with chronic health conditions who do not require intensive nursing care. Emphasis is placed on safety, mobility, and dignity, with spaces designed to feel more residential.
Common features include:
Private or semi-private rooms
Communal dining and activity areas
Support for medication, hygiene, and mobility
Emergency alert systems in resident rooms
6. Intermediate Care Facilities (ICFs)
ICFs provide long-term care and health-related services to individuals with intellectual or developmental disabilities. These facilities emphasize both medical oversight and support for independent living skills.
Services typically include:
Basic medical monitoring
Behavioral and occupational therapy
Educational and social programming
Residential accommodations
Each of these facility types has specific infrastructure needs shaped by its clinical functions, resident populations, and operational scale. As the article progresses, we will explore how electrical conduit systems are planned and implemented to support these environments safely, efficiently, and in full compliance with applicable standards.
Why Electrical Conduit Matters in Health Care Facilities

Health care environments demand exceptional electrical reliability. From advanced imaging systems to life-sustaining devices and facility-wide HVAC operations, nearly every aspect of a modern medical center relies on uninterrupted electrical power. In this high-stakes setting, electrical conduit is more than just a protective channel for wires, it is an essential infrastructure component that supports safety, continuity, and adaptability across all departments and systems.
1. Protecting Vital Medical and Support Systems
Modern health care facilities are powered by a wide spectrum of critical equipment:
- Life-support machines and surgical devices
- Imaging and diagnostics systems (e.g., MRI, CT, lab automation)
- Sterilization units and water purification systems
- HVAC systems controlling temperature, pressure, and infection control
These systems operate continuously and must be shielded from mechanical impact, chemical exposure, and environmental stress. Electrical conduit provides this protection, ensuring that cables remain undamaged, dry, and stable under various conditions.
Beyond patient-facing tools, supporting infrastructure like HVAC and water treatment also play a vital role in patient safety. A ventilation failure, for example, could compromise air quality in operating rooms, while an electrical fault in a water system could trigger pressure changes that release biofilms or contaminants.
2. Mitigating Electrical Hazards
Electrical hazards in health care settings are uniquely dangerous due to:
The density of electrical devices
Continuous human occupancy
The vulnerability of patients with limited mobility or awareness
Risks include electrical fires, shock, system malfunctions, and equipment downtime. Conduit mitigates these hazards by:
Physically shielding conductors from damage
Preventing wire exposure in high-traffic or wet environments
Controlling EMI (electromagnetic interference) near sensitive devices
In environments where even a brief outage can result in medical delays or life-threatening interruptions, proper conduit installation becomes a critical first line of defense against electrical failure.
3. Ensuring Operational Resilience
Hospitals and clinics cannot afford downtime. Separate, independent electrical systems are required, such as:
Life safety branch (emergency egress lighting, fire alarms)
Critical branch (patient monitors, ventilators)
Equipment branch (elevators, imaging equipment)
These systems must switch over to emergency power within seconds of a grid outage. Electrical conduit, especially when designed for redundancy and fire resistance, ensures that emergency feeders and backup systems remain intact and functional even under adverse conditions.
4. Adapting to Evolving Medical Technologies
The health care sector is continually evolving. Facilities must be able to accommodate:
New medical equipment (robotic surgery, AI diagnostics)
Infrastructure expansion (new wings, labs, or exam rooms)
Technological upgrades (IoT networks, EV charging for ambulances)
Power demand increases due to digital systems
Conduit systems that are properly planned and enable smooth retrofitting, expansions, and technology rollouts, without needing full system rework. This supports long-term operational flexibility and capital efficiency.
Code Compliance for Electrical Conduit in Medical Centers

In health care environments, electrical conduit systems are not just about protection and routing, they are part of a strict regulatory framework designed to ensure patient safety, system reliability, and facility integrity. Electrical engineers, designers, and contractors must follow national and regional codes that dictate what types of conduit are allowed, how systems must be grounded, and how circuits are to be isolated and protected.
The most relevant standards globally include:
- NEC (NFPA 70, U.S.) – Article 517
- CEC (Canadian Electrical Code) – Section 24
- AS/NZS 3000 / AS/NZS 3003
Below is an overview of these key code requirements:
Conseils de pro : Want to know more about PVC conduit, electrical code compliance expert insights? You can click the link below to read the electrical code compliance in your country.
NEC Code Compliance Tips (NFPA 70, USA)
Canadian Electrical Code Expert Insights (CSA Group, Canada)
National Electrical Code (NEC) – Article 517
The National Electrical Code (NEC), Article 517 is the primary authority governing electrical systems in U.S. health care facilities. It sets detailed installation criteria for hospitals, outpatient clinics, nursing homes, limited care facilities, and other settings that provide medical services to human beings.
Electrical conduit systems play a crucial role in fulfilling NEC’s aims: minimizing shock hazards, ensuring continuity of critical operations, and maintaining system grounding integrity.
Here’s a focused overview of the most important conduit-related provisions:
1. Approved Wiring Methods and Conduit Types
Metallic conduit systems (e.g., EMT, IMC, RMC) are required for branch circuits in patient care areas.
Nonmetallic conduit (e.g., PVC) cannot be used in these spaces unless encased in concrete and paired with an insulated equipment grounding conductor.
Flexible metallic conduit (FMC) may be used in limited cases, such as short connections to movable equipment.
2. Mandatory Redundant Grounding
To reduce voltage differences that can cause electric shock:
- All branch circuits must include an effective ground-fault path via the metal conduit or metallic cable armor that qualifies as an EGC.
- Additionally, an insulated copper equipment grounding conductor (EGC) must be installed with the circuit conductors.
- This dual-path requirement ensures redundant, low-impedance grounding and is mandatory for all receptacles, metal boxes, and fixed equipment in patient care areas.
Note: PVC conduit alone does not meet the dual grounding requirement and should not be used in patient care spaces unless it meets exception criteria (e.g., concrete-encased runs outside patient areas).
3. Ground-Fault Protection Requirements
Critical care hospitals and facilities with life-support systems must install ground-fault protection on main service and feeder disconnects to reduce arc flash and fire risk.
4. Receptacles at Patient Bed Locations
Minimum receptacles: 8 for general care; 14 for critical care areas per patient bed location.
Must include devices on both normal power and critical branch circuits.
Receptacles must be:
Hospital-grade
Individually grounded via insulated copper EGC
Clearly marked to show panel and circuit origin
5. Essential Electrical System (EES)
Healthcare facilities are required to maintain a multi-branch emergency electrical system, designed to operate during power outages. This is essential for life safety and to prevent disruption to critical operations.
The code requires three separate branches:
Life Safety Branch: Egress lighting, fire alarms, communication.
Critical Branch: Equipment directly supporting patient care (monitors, ventilators).
Equipment Branch: HVAC, imaging, pumps.
Each branch must:
Be powered by separate panelboards and transfer switches.
Use dedicated conduit and raceways, no mixing of circuits.
Be mechanically protected and comply with 517.13 grounding rules in patient spaces.
6. Wet Procedure Locations
Requires shock protection in wet procedure locations (e.g., ORs with washdown), using either:
Isolated power systems or leakage interruption systems.
7. Bonding, Junctions, and Connections
517.13 and 517.19(E) specify approved methods for bonding metal raceways:
- Grounding bushings
- Threaded hubs
- Bonding-type locknuts or bushings
Ensures continuity of the EGC across all junction points.
8. Special Locations (Anesthesia, X-ray, Data, and Fire Alarms)
Article 517 classifies flammable anesthetizing locations as Class I, Division 1 hazardous.
And for Low-voltage systems (e.g., nurse call, fire alarms, signaling) in patient care areas, requiring equivalent insulation and separation but are exempt from full conduit/grounding mandates unless otherwise noted.
NEC Article 517 is one of the most comprehensive and stringent sections of the Code. Its goal is not just to protect systems, but to protect lives – patients, clinicians, and staff, by ensuring electrical integrity in the most sensitive environments. Electrical conduit is at the heart of this strategy, providing both mechanical protection and grounding infrastructure for critical health care circuits.
Canadian Electrical Code (CEC) – Section 24
In Canada, electrical installations in health care settings are regulated by the Canadian Electrical Code (CEC), Section 24: Patient Care Areas. This section outlines specific safety and performance standards for hospitals, clinics, long-term care facilities, and other medical environments where patients may be examined, diagnosed, or treated.
Section 24 imposes special rules beyond general electrical practices, focusing on branch circuit design, grounding and bonding, essential electrical systems, and isolation techniques. These rules aim to reduce the risk of electrical shock, ensure system reliability during emergencies, and protect both patients and healthcare personnel.
1. Designation of Care Areas
CEC Section 24 applies to three types of patient care areas:
- Basic Care Areas (e.g., general treatment rooms)
- Intermediate Care Areas (e.g., intensive monitoring wards)
- Critical Care Areas (e.g., ICUs, operating rooms)
These categories determine the stringency of electrical protection and conduit requirements.
2. Branch Circuit Requirements in Patient Care Environments
- All branch circuits must use copper conductors, not smaller than No. 12 AWG.
- Circuits must originate from a grounded distribution system, or in some cases (critical/intermediate care), from isolated power systems.
- Circuits supplying receptacles or equipment in a patient care environment must not serve loads outside that space, except for adjacent rooms, with proper restrictions.
- Circuits must be limited to 150 V to ground, unless supplying specialized medical equipment like mobile X-ray units.
3. Bonding and Grounding in Patient Care Areas
Proper bonding to ground is mandatory to ensure all accessible conductive surfaces are at the same potential, minimizing shock hazard.
Key conduit and wiring requirements include:
- Insulated bonding conductors must be used, except when in non-metallic conduit or appropriate cable assemblies.
- Every branch circuit must include a dedicated equipment bonding conductor, even in multi-wire arrangements.
- Bonding conductors must run with the circuit conductors inside the same raceway or cable.
- Panelboards serving these circuits must be bonded using copper conductors sized per CEC Table 16, and not smaller than No. 6 AWG when bonding between multiple panels.
- Three-phase equipment and exposed conductive parts of medical/non-medical systems must be bonded with individual conductors.
Conduit systems (metallic or non-metallic) play a vital role in mechanically protecting bonding paths and maintaining proper separation between grounded and isolated systems.
4. Receptacle Requirements
All 15 A and 20 A non-locking receptacles must be hospital grade (except for housekeeping use).
Receptacles powered by essential electrical systems must be red-colored for identification.
Isolated ground receptacles are not permitted in any patient care area.
In areas cleaned with liquids or subject to flooding, receptacles must be:
At least 300 mm above floor level, and
GFCI-protected or supplied from an isolated system.
5. Essential Electrical Systems (EES)
CEC mandates that healthcare facilities have an essential electrical system that continues to function during a utility power outage. It ensures that life safety, critical medical equipment, and facility operations are not interrupted.
Key components include:
Vital Branch: Supplies life-support and patient-care equipment.
Delayed Vital Branch: Supports loads that can be reconnected with a short delay.
Conditional Branch: Supplies other important, but not life-critical, loads.
Conduit and wiring for EES must:
Be physically separated from all non-essential systems.
Be installed in dedicated raceways, boxes, and cabinets, with exceptions only for transfer switches or dual-fed emergency lights.
Include automatic or manual transfer switches, which must comply with CSA standards.
Emergency power must be provided by:
On-site generator sets.
Installed in a service room or enclosure compliant with fire and mechanical codes.
6. Isolated Power Systems in Critical and Wet Areas
For certain critical care or wet procedure locations, isolated power systems are required to:
Limit the current-to-ground during a first fault.
Avoid circuit tripping and allow continuous equipment operation while maintaining safety.
Core requirements:
Supplied by isolating transformers, motor-generators, or battery inverters.
Include line isolation monitors with visible alarms.
Conductor insulation must be color-coded (e.g., orange and brown) and meet specific dielectric performance standards.
Only single or adjacent rooms may be supplied per isolated circuit to maintain fault identification.
Note: Grounded and isolated circuits must not share the same conduit, even if separated internally.
AS/NZS 3000 and AS/NZS 3003

In Australia and New Zealand, electrical installations in health care facilities are governed by a two-tiered framework consisting of AS/NZS 3000:2018 and AS/NZS 3003:2018:
- AS/NZS 3000 (Règles de câblage) establishes general requirements for safe electrical installations across all types of buildings and occupancies.
- AS/NZS 3003: Electrical installations—Patient areas supplements these rules with specific provisions for electrical installations in patient areas of healthcare facilities, where safety is paramount due to direct patient interaction with electrical medical equipment.
AS/NZS 3000: General Wiring Rules
AS/NZS 3000 is the base document for all low-voltage electrical installations in Australia and New Zealand. Although it is not healthcare-specific, it forms the legal and technical foundation for:
- Selection of wiring systems and conduit types,
- Installation methods and clearances,
- Earthing, bonding, and circuit protection,
- Segregation of services (power, control, communication),
- Protection against electric shock, fire, mechanical damage, and undervoltage, and
- Inspection and testing requirements.
AS/NZS 3003: Patient Areas
AS/NZS 3003 applies specifically to “patient areas”, defined as spaces where electrical equipment may be used in contact with patients during diagnosis, monitoring, or treatment. This includes:
General medical/surgical wards,
Emergency departments,
Intensive care units (ICUs),
Operating theatres,
Recovery rooms,
Dialysis and oncology treatment zones,
Cardiac catheter labs, and
Aged care rooms with medical support.
AS/NZS 3003 distinguishes two protection categories:
- Body-protected areas: where electrical contact with the body is possible (e.g., general wards).
- Cardiac-protected areas: where equipment may affect heart function or pose life-critical risks (e.g., ICUs, theatres).
Key Requirements of AS/NZS 3003 Code:
Wiring and Distribution
No looping: Each socket-outlet must be wired on a dedicated final subcircuit—no daisy-chaining.
Circuits must originate from the same distribution board serving that patient area.
Circuit protection must avoid shared neutrals in patient areas to prevent shock risks and ensure isolation.
Colour coding is required for medical socket-outlets (e.g., red or green) to denote function and supply.
Socket-Outlets (Receptacles)
Only hospital-grade socket-outlets may be used.
Isolated-ground (IG) outlets are not permitted in patient areas due to the increased risk of electric shock under certain fault conditions.
All socket-outlets must be clearly labeled and traceable to the supplying circuit and protection device.
Equipotential Bonding and Earth Reference
Supplementary equipotential bonding is required in both body- and cardiac-protected areas.
Bonding conductors must connect all exposed conductive parts, such as medical equipment housings, patient bed rails, metallic pipes, and gas outlets, to a common earth reference bar (ERB).
Bonding is crucial for minimizing touch voltages and preventing dangerous potential differences during faults or leakage.
Isolated Power Systems (IPS)
In cardiac-protected areas, an Isolated Power Supply (IPS) is typically required to limit fault current and maintain continuity of supply during a single fault condition.
The IPS must include:
Line Isolation Monitor (LIM) that alerts staff to insulation faults,
Separate supply via isolating transformers, and
Insulation monitoring that complies with Class 1 equipment use.
IPS circuits must be single-phase, 2-wire, and identified with orange and brown conductors.
Protection Devices and Residual Current Devices (RCDs)
RCDs are required for general-purpose socket-outlets but must not be used where they could interrupt power to life-support equipment without medical approval.
Special consideration is required for selective coordination and time-delay RCDs in essential circuits.
RCD protection may be omitted in certain IPS or isolated medical systems.
Inspection and Testing
AS/NZS 3003 outlines detailed initial verification and periodic testing protocols, including:
Earth fault loop impedance,
Insulation resistance,
Polarity,
Operation of RCDs and LIMs,
Continuity of protective earth and bonding systems.
Testing must be documented and repeated periodically to ensure ongoing safety and compliance.
Conduit and Cabling
Metallic and non-metallic conduit systems must provide mechanical protection and support fault loop impedance requirements.
Segregation is mandatory between different systems (e.g., power, data, nurse call, and emergency lighting).
All cables must be low-smoke and halogen-free where required by local fire codes or healthcare policy.
Installation & Maintenance of Electrical Conduit in Health Care Facilities

Proper installation and diligent maintenance of electrical conduit systems are fundamental to ensuring electrical safety, reliability, and compliance within health care environments. Given the unique risks present in patient care areas, such as critical equipment loads, life support systems, and restricted evacuation capabilities, conduit systems must be installed to the highest standard, with ongoing maintenance tailored to prevent faults and downtime.
This section explores best practices and key considerations for installing and maintaining conduit systems in hospitals, clinics, nursing homes, and other medical facilities.
Installation Best Practices
1. Material Selection by Zone
Health care facilities contain a wide variety of spaces, each with specific electrical and environmental requirements. Conduit material should be selected based on:
Patient care areas (basic, intermediate, critical): Often require metallic conduit (e.g., EMT, RMC) for effective grounding.
MRI or imaging suites: Prefer non-metallic conduit (e.g., PVC or fiberglass) to avoid electromagnetic interference.
Operating theatres and wet procedure areas: Require enhanced sealing, corrosion resistance, and mechanical strength, PVC-coated steel conduit is commonly used.
2. Segregation and Raceways
As required by codes:
Essential system conduits (life safety, critical care) must be installed independently from non-essential wiring.
Avoid sharing raceways, junction boxes, or panels across different electrical systems.
Use color-coded conduits or labels to distinguish normal, critical, and emergency power circuits.
3. Grounding and Bonding
Grounding is vital to patient safety and is rigorously regulated. Conduit systems must:
Ensure continuous electrical continuity (especially in metallic systems).
Be installed with equipment grounding conductors (EGC) where required, particularly in patient care areas.
Follow specific bonding requirements, including minimum conductor sizing and dedicated bonding points.
4. Sealing and Infection Control
Conduit penetrations in walls and ceilings should be:
Properly sealed using firestopping materials approved for electrical penetrations.
Designed to prevent fluid ingress in procedure rooms or damp environments.
Installed in a way that minimizes dust accumulation and supports hygienic surfaces.
5. Support and Accessibility
All conduit runs must be:
Securely supported at regular intervals to prevent sagging or movement.
Installed to allow access to junctions and pull points for inspection and cable replacement.
Routed to avoid overhead obstructions, medical gas lines, or patient bed areas unless protected.
Maintenance and Inspection Requirements
1. Routine Visual Inspections
Facility engineers or electrical contractors should perform routine visual checks, ideally semi-annually or annually, to look for:
Conduit damage (cracks, corrosion, dents)
Disconnected fittings or loose supports
Water or fluid intrusion into boxes or raceways
Obsolete markings or missing identification
2. Testing of Grounding and Bonding
Regular verification of bonding integrity is essential:
Measure continuity between equipment grounding conductors and bonding points in patient care spaces.
Confirm that metallic raceways still provide an effective fault current path.
Inspect grounding of receptacles and panels, especially after system upgrades.
3. Environmental Monitoring
Conduit systems in harsh environments (e.g., HVAC rooftops, boiler rooms, sterilization areas) must be checked for:
UV degradation of plastic conduits
Corrosion in metallic conduit systems
Mechanical wear from vibration or impacts
4. Upgrades and Retrofits
When new medical equipment is introduced, conduit systems may need:
Re-routing or upsizing to meet ampacity and bend radius requirements.
Rebonding to maintain ground-fault protection.
Reclassification of areas (e.g., general to critical care), requiring conduit upgrades to meet stricter installation standards.
5. Record Keeping and Compliance Audits
Accurate documentation supports code compliance and operational continuity:
Maintain as-built conduit layout drawings and circuit schedules.
Keep records of inspection dates, deficiencies, repairs, and test results.
Ensure the facility is ready for compliance audits from local electrical authorities or accreditation bodies.
Remarques : Want to know the detailed steps and expert tips for installing electrical conduit? You can click on the above link to read our last post.
Conclusion
In health care environments, where electrical reliability is inseparable from patient safety, conduit systems are far more than passive infrastructure—they are essential components of a life-critical ecosystem. From supporting vital equipment and emergency systems to meeting stringent code requirements across the U.S. (NEC), Canada (CEC), and Australia/New Zealand (AS/NZS), conduit plays a foundational role in protecting circuits, preventing hazards, and enabling operational resilience.
In all, the role of electrical conduit in health care goes far beyond containment. It is a silent yet essential guardian of safety, performance, and resilience, forming the backbone of electrical systems in environments where failure is not an option.
FAQ :
What is the primary purpose of electrical conduit in healthcare facilities?
Electrical conduit protects wiring systems from physical damage, supports essential services like power, lighting, medical equipment, and communication, and helps ensure uninterrupted operation of life-critical systems. It also enables proper grounding, isolation, and fire containment, essential in environments with vulnerable patients and sensitive electronics.
Why are electrical safety standards so strict in healthcare environments?
Patient safety is paramount. In medical settings, even minor electrical faults can cause injury, equipment failure, or fatal outcomes. Strict standards minimize risks of electrical shock, fire, electromagnetic interference, and system outages, especially around life-support devices and patient care areas.
What types of electrical conduit are typically permitted in healthcare settings?
Permitted conduit types include:
Metallic Raceways (EMT, RMC, IMC) – for patient care areas to ensure grounding integrity.
Flexible Metallic Conduit (FMC) – for equipment connections, with limitations.
Nonmetallic conduit (e.g., PVC) – may be used outside patient care areas or with proper grounding and protection.
What are some common electrical hazards in healthcare facilities that robust conduit helps mitigate?
Electrical shock in patient care spaces
Short circuits and arcing
Overheating and wire damage
Power failure of life-support equipment
Cross-interference in sensitive equipment
Fire propagation in cable routes
What is the meaning of EES in electrical?
EES stands for Essential Electrical System, which is a dedicated part of a healthcare facility’s power infrastructure designed to operate during a utility outage. It ensures continuity of patient care and safety-critical systems during emergencies.
What are the different types of EES?
In hospitals, the Essential Electrical System (EES) typically includes:
Life Safety Branch – Emergency lighting, fire alarms, and egress systems.
Critical Branch – Circuits for patient life-support, medical equipment, and critical operations.
Equipment Branch – HVAC, pumps, and building systems essential for operation.
What is the earthing system in a hospital?
Hospitals use a robust equipotential grounding and bonding system to maintain low impedance paths and minimize voltage differences in patient care areas. It includes:
Grounded distribution systems
Equipment bonding conductors
Isolated ground networks in specific zones
Centralized grounding points (e.g., patient equipment grounding terminals)
Are Residual Current Devices (RCDs) mandatory in Australian/New Zealand healthcare facilities?
Yes, RCDs are required in wet areas or where floor fluids may present shock hazards. AS/NZS 3003 mandates RCD protection or isolated power systems (with Line Isolation Monitors) in such high-risk locations to prevent electrocution and ensure continuous operation.
What are the fire protection requirements for healthcare facilities?
Fire protection includes:
Metallic conduit to contain electrical fires
Hospital-grade fire-stopping at penetrations
Redundant EES for evacuation lighting and alarms
LSZH cables and conduit to reduce toxic smoke
What is the most common cause of fires in hospitals?
Electrical faults (short circuits, arcing, overloaded circuits) are among the leading causes of hospital fires, especially near high-load equipment and older infrastructure.
Can I use PVC conduit in health care facility installations?
Yes, PVC conduit is allowed outside patient care areas, in non-critical zones, or for underground and feeder runs. However, it must not be used in patient care spaces unless accompanied by a separate insulated grounding conductor and complying with NEC 517.
Do hospital conduits need to be grounded?
Absolutely. All conduit systems in patient care areas must ensure effective equipment grounding. Metallic conduits often act as grounding paths; where nonmetallic is used, a separate insulated copper ground is required.
Can flexible conduit be used in hospitals?
Yes, but with limitations. Flexible Metal Conduit (FMC) or Liquid-tight Flexible Metal Conduit (LFMC) may be used for final connections to equipment but must comply with NEC/CEC/AS/NZS installation practices and not be used as the primary wiring method in patient areas.
Is conduit required for fire alarm and emergency lighting in hospitals?
Yes. Fire alarm and emergency lighting circuits in healthcare settings are considered life safety systems and typically must be run in metallic conduit (EMT/RMC) or fire-rated assemblies to ensure durability, separation, and compliance with codes.




